Glucagon-like peptide 1 (GLP-1) in the treatment of Diabetes
Type 2 diabetes is a major risk factor for cardiovascular disease related morbidity and mortality. There are several therapies for the management of type 2 diabetes, but still optimal glycemic control is not achieved in spite of advances in options for the treatment of diabetes. A large number of patients fail to attain the glycemic target and only few drugs have shown to effectively control the Hb1Ac numbers below <7%. The biggest hurdles for the implementation and long term application of intensive therapies are the low blood sugar levels (hypoglycemia) and weight gain. Currently available drugs act to increase insulin availability through administration, secretion or by increasing sensitivity. Others act by delaying the delivery and absorption of carbohydrate from the gastrointestinal tract, or by increasing urinary glucose excretion. There still seems to be an unmet need in this therapeutic area, in spite of these drugs on the market. Recently there have been advances in type 2 diabetes management in the clinical development of dipeptidyl peptidase-4 (DPP-4) inhibitors and in glucagon-like peptide 1 receptor agonists. (1)
Glucagon-like peptide 1 (GLP-1) belongs to the hormonal family of incretins that enhance the secretion of insulin. Incretins are a group of gastrointestinal hormones that stimulate lower blood glucose levels by increasing the amount of insulin released from pancreatic beta cells. The two primary incretin hormones are glucagon like peptide GLP-1 and GIP (gastric inhibitory polypeptide or glucose-dependent insulinotropic polypeptide). Both GLP-1 and GIP are rapidly cleaved by dipeptidyl peptidase-4 (DPP-4). GLP-1 is a product of a precursor molecule called pre-proglucagon, a polypeptide which is split to produce many hormones including glucagon. As they have same origin, these hormones share some similarities, and hence the name ‘glucagon-like’.
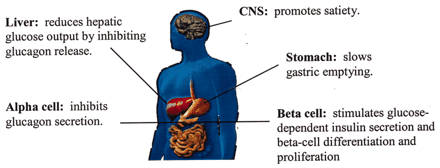
The major sources of GLP- 1 are the L-cells in the lining of small intestine. The pancreas and the central nervous system (CNS) also secrete this hormone in smaller quantities. GLP- 1 stimulates the release of insulin from the pancreas; it also increases the volume of cells in the pancreas which produces insulin (beta cells) and regulates and controls the release of glucagon. GLP-1 acts on appetite centers in brain, slowing the emptying process in stomach and increasing the feeling of fullness during and between the meals. (2)
Differential processing of proglucagon in the intestinal epithelial endocrine L-cells produces the 30-amino acid peptide hormone GLP-1. The metabolism of GLP-1 in the body is extremely rapid and the peptide gets inactivated by the enzyme dipeptidyl peptidase-4 (DPP-4), even before leaving the gut. (3). Glucagon is a key hormone in glucose metabolism and homeostasis. It regulates blood glucose by decreasing glycolysis and increases the rate of gluconeogenesis. It counter-regulates the hormone of insulin by raising plasma glucose levels in response to insulin-induced hypoglycemia. Glucagon is known to play an important role in initiating and maintaining hyperglycemic conditions in diabetes and to suppress the plasma glucagon level. (4)
It is assumed that GLP-1 may be involved in the stimulation of glucose disposal in peripheral tissues independent of insulin actions.
Clinical Diabetes, April 2005 vol. 23 no. 2 56-62
Figure 1.Multiple sites of action for GLP-1. Image courtesy: American Diabetes Association and Dr. John. Buse MD, PhD.
GLP-1 and GLP-2 stimulate intestinal growth and upregulate villus height in the gastrointestinal tract. The primary site of action of GLP-2 starts in the stomach and ends in the colon. It has an essential function in nutrient homeostasis (5) by an increased stimulus in the gastrointestinal track which leads to an increment in nutrient assimilation. The Pharmaceutical industry has developed drugs that mimic the GLP-1 targeting control of glucose levels in type-2 diabetes. Weight loss contributes in increasing the GLP-1 levels leading to improved glucose control in Type-2 Diabetes. Lower levels of GLP-1 in the body lead to obesity, feeling of hunger and empty stomach making the individual eat more.
Incretin based GLP-1 therapies have additional effects, e.g. the reduction of glucagon, the slow down of gastric emptying, and inducing the sense of satiety. In clinical practice these therapies are associated with significant reductions in glycated hemoglobin (HbA1c) weight loss and a low risk of hypoglycemia. Few of the incretin GLP-1 receptor agonist based therapies are mentioned below:
Exenatide (exendin-4) is a reptilian hormone isolated from the saliva of the Gila monster (Heloderma suspectum) which acts as a GLP-1 mimic. The 39 amino acid-containing peptide has been approved as a monotherapy for the treatment of type-2 diabetes.
Exenatide is marketed under the trade name of Byetta® by AstraZeneca. It enhances insulin production and has 53% sequence identity to GLP-1. Because of its shorter half-life of 2.4 hours exenatide has twice-a-day dosing regimen taken with metformin ± sulfonylurea. Exenatide was well tolerated in patients and rates of hypoglycemia were relative low in these studies.
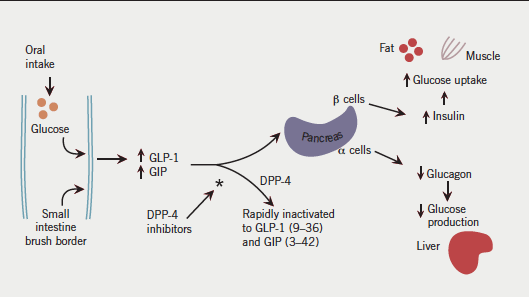
Oral glucose stimulates the release of the endogenous incretins glucagon-like peptide-1 (GLP-1) and glucose-dependent insulin-releasing polypeptide (GIP). These stimulate insulin release and inhibit glucagon release resulting in lower blood glucose. They are rapidly inactivated by dipeptidyl peptidase-4 (DPP-4). The DPP-4 inhibitors prolong the action of endogenous incretins, enhancing the first-phase insulin response. (Image courtesy: Dr.Fisher Miles).
Liraglutide is a GLP-1 analog which has 97% sequence -similarity towards GLP-1. It is marketed under the trade name Victoza® by Novo Nordisk. The fatty acid side chain enables the heptamer formation thus increasing the stability and the binding to albumin. The drug was generally well tolerated and rates of hypoglycemia seemed to be low in these trials; however frequency of hypoglycemia increased with the combined use of other anti-diabetic drugs (metformin and sulfonylurea drugs). It was reported that in direct comparison between exenatide twice daily and liraglutide once a day, liraglutide was significantly more effective in controlling the glycemic index when compared to exenatide. The weight and fasting plasma glucose was significantly reduced by liraglutide treatment.
Exenatide LAR from Amylin/ AstraZeneca: A once-weekly injection of exenatide has been approved as of January 27, 2012 under the trademark Bydureon®. Exenatide once a week dose was more effective when compared to twice a day dose of exenatide.
| Drug Name | Developer/Manufacturer | Dosage | Plasma Half life | Approval year/Countries |
|---|---|---|---|---|
| Exenatide | AstraZeneca | 5-10 mcg SC route | 2.4 hrs | 2005 USA |
| Liraglutide | Novo Nordisk | 1.2-1.8 mg once SC | 11-15 hrs | 2009 USA |
| Taspoglutide | Ipsen/Roche | -- | 165 hrs | |
| Lixisenatide | Sanofi-Aventis | 20 mcg daily | 2.7-4.3 hrs | EU, Mexico, Australia, Japan |
| Semaglutide | Novo Nordisk | TBD | 160hrs |
Table showing the list of GLP-1 Receptor Agonist: Adapted with permission from J. Med. Chem., Article ASAP. DOI: 10.1021/jm500810s.Publication Date (Web): October 28, 2014 Courtesy: copyright 2014; American chemical society.
In hypoglycemia, GLP-1 reduces the brain glucose concentration. Further effects are an increase of the net blood brain clearance and the brain metabolism, but it is not known whether they depend on the prevailing plasma glucose (PG) (6). GLP-1 peptide is a post- translational product of preglucagon which is a precursor of many glucagon related peptides. They are two equipotent forms of GLP-1, GLP-1 (7-36)-NH2 and GLP-1 (7-37), the first one being more abundant, which bind to and activate the GLP-1 receptor. The GLP-1 receptor or GLP-1R belongs to the class B family of G-protein coupled receptors (GPCRs) and carries out its regulatory functions. GLP-1R is found in many organs like pancreas, kidney, GI tract and brain, but is highly expressed in pancreas.
In summary it is projected that GLP-1 agonist peptides against type-2 diabetes are promising targets for patients with poor Hb1Ac control.
References:
1. Anon., Lancet 1998, 352, 837.
2. Stephen Bloom et.al; Imperial College London Society of Endocrinology; BES 2013.
3. J. J. Holst, Physiol Rev 2007, 87, 1409.
4. S. Runge, B. S. Wulff, K. Madsen, H. Brauner-Osborne, L. B. Knudsen, Br J Pharmacol 2003, 138, 787.
5. C. X. Dong, P. L. Brubaker, Nat Rev Gastroenterol Hepatol 2012, 9, 705.
6. M. Gejl, S. Lerche, L. Egefjord, B. Brock, N. Moller, K. Vang, A. B. Rodell, B. M. Bibby, J. J. Holst, J. Rungby, A. Gjedde, Front Neuroenergetics 2013, 5, 2.
